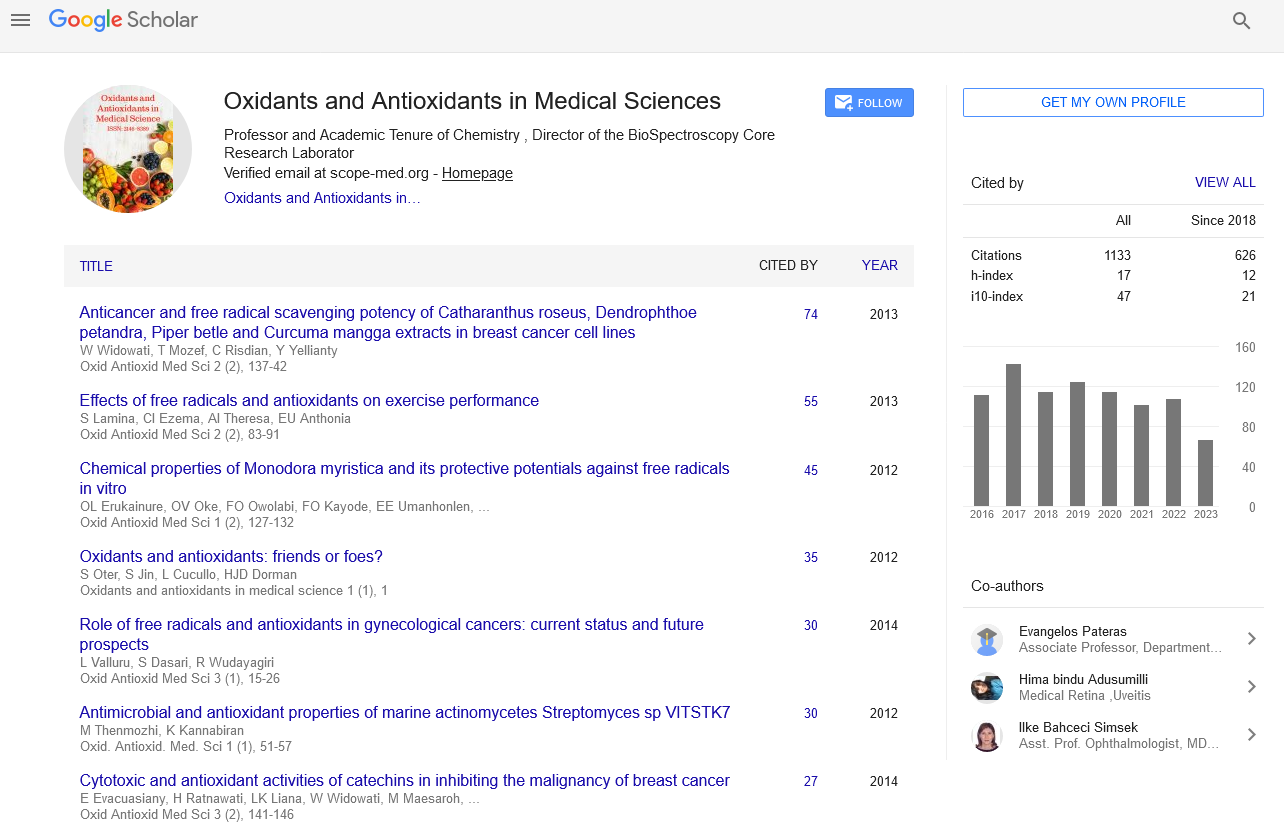
Commentary - Oxidants and Antioxidants in Medical Science (2022)
A Brief Note on Mitochondrial Sources of Reactive Oxygen Species (ROS) and Reactive Nitrogen Species (RNS)
Pault Mour*Pault Mour, Department of Chemical Engineering, University of Tehran, Tehran, Iran, Email: pautmour@gmail.com
Received: 29-Nov-2022, Manuscript No. EJMOAMS-22-82536; Editor assigned: 02-Dec-2022, Pre QC No. EJMOAMS-22-82536 (PQ); Reviewed: 19-Dec-2022, QC No. EJMOAMS-22-82536; Revised: 26-Dec-2022, Manuscript No. EJMOAMS-22-82536 (R); Published: 02-Jan-2023
Description
Reactive Oxygen Species (ROS) and Reactive Nitrogen Species (RNS) serve important physiological functions but can also cause significant cellular damage in a balance determined by their relative rates of generation and removal. These species are usually removed quickly before they cause cellular dysfunction and death. Oxidative/nitrosative stress caused by an imbalance between ROS/RNS generation and antioxidant defense capacity can affect major cellular components including lipids, proteins, carbohydrates, and DNA. Mitochondria are recognized as a critical site in the cell for ROS/RNS generation and targeting.
Mitochondrial sources of ROS
It is generally accepted that mitochondria are the main source of ROS in the cell. These organelles contain several enzymes that catalyse the formation of ROS, either as an obligatory product or as an incidental, perhaps unwanted, reaction. The best example of “accidental” formation of ROS is the mitochondrial respiratory chain. A small fraction of the electrons (about 0.1%) passing through the respiratory chain are withdrawn, causing partial reduction of O2 to superoxide. This process occurs at the level of the first three complexes, where flavins or quinones are able to act as single electron donors [1].
Mitochondria also contain other enzymes that can generate hydrogen peroxide (H2O2) as a direct and obligatory product. One such example is a cytosolic adapter protein that, under stress, trans-locates to the mitochondria where it catalyzes the transfer of electrons from cytochrome c to oxygen, a process that can lead to the formation of ROS. Genetic deletion protects against I/R injury in mice, obesity, and diabetic complications such as cardiomyopathy, nephropathy, delayed wound healing, pancreatic cell death, and endothelial dysfunction [2]. On the other hand, the observation that null mice actually live shorter when exposed to natural conditions (low temperatures and food competition) may suggest that dependent ROS also play a physiological role. NADPH oxidase 4 (Nox4), an enzyme belonging to the NADPH oxidase family, is another ROS-generating enzyme that has been reported to localize to the plasma membrane and apparently also to mitochondria, focal junctions, the nucleus and endoplasmic reticulum. This enzyme binds to for its activation; it is constitutively active and, unlike other Nox family members, generates H2O2 rather than superoxide. However, the significance of Nox4 for mitochondrial ROS generation remains controversial [3].
A recent study showed that Nox4 can interact with complex I subunits, but under physiological conditions Nox4 protein or ROS formation cannot be detected in kidney and heart mitochondria. Other studies have shown that specific targeting of Nox4 to the heart can be both protective and deleterious in various models of cardiac pressure overload. Moreover, while some studies have reported that Nox4 is detrimental, contributing to mitochondrial dysfunction and several pathologies such as ischemic stroke, diabetic cardiomyopathy, and vascular inflammation and remodelling, others have concluded that Nox4 may protect the vasculature rather than harm them [4]. These apparently conflicting findings reflect the need for further investigation in order to resolve the pathophysiological role and regulation of Nox4. Another main source of H2O2 in Mitochondria is Monoamine Oxidase (MAO). Activation of this enzyme, localized at the level of the OMM, leads to the formation of H2O2 and has been shown to contribute to neuronal disorders such as Parkinson’s disease or Alzheimer’s disease, most likely due to the formation of ROS responsible for oxidative damage to neurons. In recent years, the contribution of MAO to oxidative stress, which ultimately leads to mitochondrial dysfunction and cell damage, has also been demonstrated in the cardiovascular field, where MAO inhibition has been shown to be protective ischemia-reperfusion injury, pressure overload, injury blood vessels and diabetes.
Mitochondrial sources of RNS
In addition to ROS, cells are also able to generate RNS. NOS exist in three isoforms, which catalyse the conversion of L-arginine to citrulline and NO. Flavinadenine dinucleotide, flavinomononucleotide, tetrahydrobiopterin, heme, and calmodulin are also required for this reaction [5]. These cofactors are important (eg, when BH4 levels are limited) because NOS can become uncoupled and generate superoxide instead of NO. Another possibility is that under conditions of high oxidative stress, NO and superoxide interacts to generate ONOO−, a highly reactive species able to nitrate tyrosine residues, thus enhancing oxidative damage [6].
It is generally accepted that NO has a protective effect on mitochondria, although it remains unclear whether mitochondria actually possess mitochondrial NOS. In any case, the biological activity of the newly synthesized NO is quickly terminated by its oxidation to and, thus completing the NO cycle. The protective effect exerted by NO on mitochondria is due to S-nitrosylation of critical cysteine residues.
References
- Sun J, Morgan M, Shen RF, Steenbergen C, Murphy E. Preconditioning results in S-nitrosylation of proteins involved in regulation of mitochondrial energetics and calcium transport. Circ Res 2007; 101(11):1155-1163.
[Crossref] [Google scholar] [PubMed]
- Sun J, Nguyen T, Aponte AM, Menazza S, Kohr MJ, Roth DM, et al. Ischaemic preconditioning preferentially increases protein S-nitrosylation in subsarcolemmal mitochondria. Cardiovasc Res 2015; 106(2):227-236.
[Crossref] [Google scholar] [PubMed]
- Das N, Jana CK. Age-associated oxidative modifications of mitochondrial α-subunit of F1 ATP synthase from mouse skeletal muscles. Free Radic Res 2015; 49(8):954-961.
[Crossref] [Google scholar] [PubMed]
- Augereau O, Claverol S, Boudes N, Basurko MJ, Bonneu M, Rossignol R, et al. Identification of tyrosine-phosphorylated proteins of the mitochondrial oxidative phosphorylation machinery. Cell Mol Life Sci 2005; 62(13):1478-1488.
[Crossref] [Google scholar] [PubMed]
- Plun-Favreau H, Burchell VS, Holmström KM, Yao Z, Deas E, Cain K, et al. HtrA2 deficiency causes mitochondrial uncoupling through the F1F0-ATP synthase and consequent ATP depletion. Cell Death Dis 2012; 3(6):e335.
[Crossref] [Google scholar] [PubMed]
- Dupuis A, Lunardi J, Issartel JP, Vignais PV. Interactions between the oligomycin sensitivity conferring protein and beef heart mitochondrial F1-ATPase. 2. Identification of the interacting F1 subunits by crosslinking. Biochemistry 1985; 24(3):734-739.
[Crossref] [Google scholar] [PubMed]
Copyright: © 2023 The Authors. This is an open access article under the terms of the Creative Commons Attribution NonCommercial ShareAlike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.