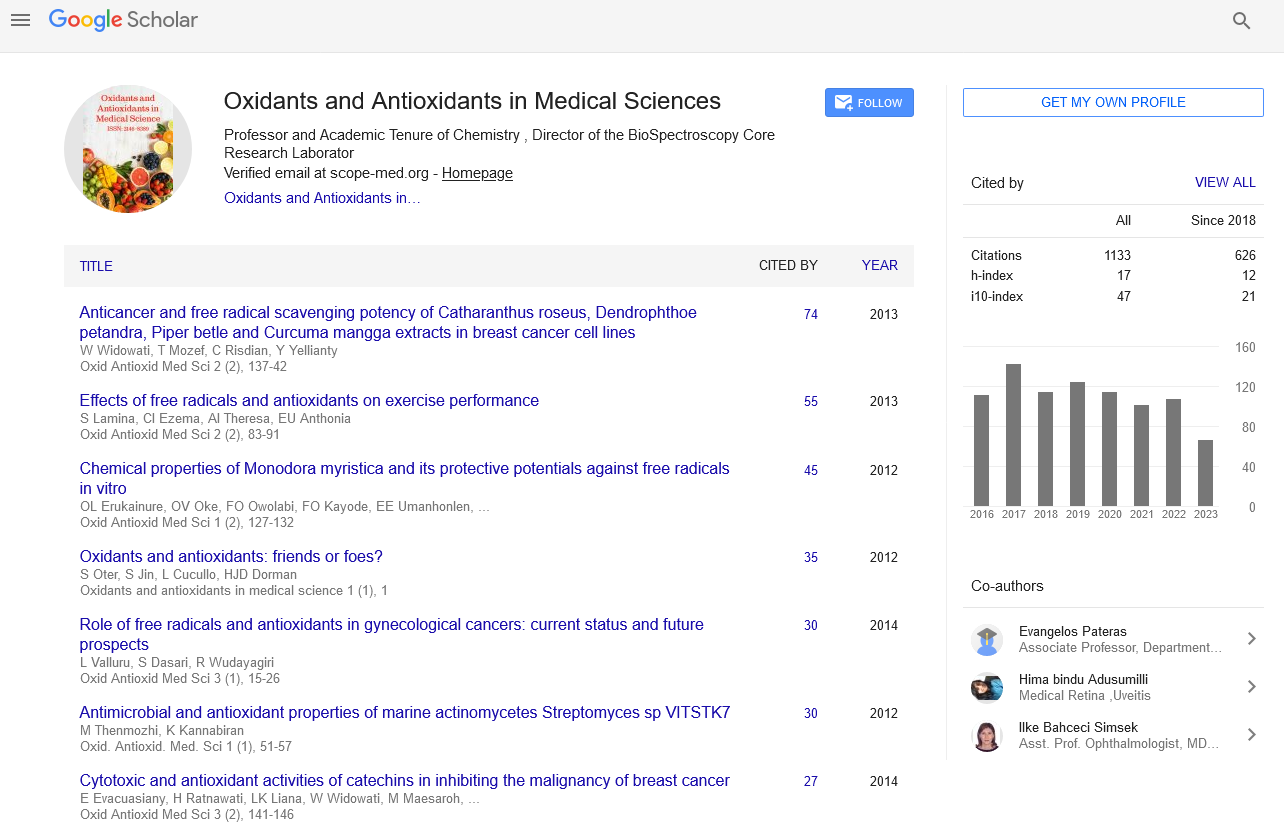
Commentary - Oxidants and Antioxidants in Medical Science (2022)
Role of Enzymatic Antioxidants in Oral Diseases
Mar Morase*Mar Morase, Department of Chemistry, University of Purnea, Purnia, Bihar, India, Email: mar.morase@hotmail.com
Received: 03-Oct-2022, Manuscript No. EJMOAMS-22-77356; Editor assigned: 07-Oct-2022, Pre QC No. EJMOAMS-22-77356 (PQ); Reviewed: 21-Oct-2022, QC No. EJMOAMS-22-77356; Revised: 27-Oct-2022, Manuscript No. EJMOAMS-22-77356 (R); Published: 03-Nov-2022
Description
A substance capable of neutralizing the harmful effects of free radicals on the human body is called an antioxidant. Antioxidants can be defined as substances that, at very low concentrations, inhibit the oxidation of any molecule. The harmful effects of free radicals obtained as metabolic products are inactivated by antioxidants. Free radicals are extremely reactive molecules that either donate or withdraw electrons from neighbouring molecules with which they react.
Different types of antioxidants are glutathione, vitamin A, vitamin E, catalase enzymes, Superoxide Dismutase (SOD), and various peroxidases. This review discusses enzymatic antioxidants and their role in oral disease. The main antioxidant enzymes highlighted in the current review are SOD, Glutathione Peroxidase (GPX), catalase [1,2].
Enzymatic antioxidants
Superoxide dismutase: Superoxide dismutase is an enzyme found throughout the body that catalyzes the dismutation of superoxide. Hydrogen peroxide is produced as a by-product of this reaction, which aids in the repair of free radical damage. The human body produces an incredible amount of reactive oxidants such as hydrogen peroxide, superoxide and hydroxyl radicals. The hydroxyl radical is the most catastrophic for tissue, causing the destruction of adjacent cells. The SOD enzyme has three variants. The predominant enzymes containing copper and zinc are found in the cytoplasm, while manganese SOD is found in the mitochondria. The third type is present extracellularly [3,4].
Glutathione: Glutathione peroxidase and glutathione reductase are enzymes that act as antioxidants. The reduced form of glutathione is protective. The oxidized form is not protective. Reduced glutathione helps neutralize hydrogen peroxide that is produced inside the cell. These enzymes are key players in preventing increased levels of oxidative stress [5]. This repeated oxidation and reduction of glutathione makes it a scavenger of free radicals [6].
Catalase: Catalase is an antioxidant enzyme that acts as a catalyst for the conversion of hydrogen peroxide into oxygen and water. It neutralizes the effect of hydrogen peroxide, which is inside the cells. The exact amount of catalase present in the cytoplasm cannot be estimated because most of it is lost during tissue manipulation.
Role of antioxidants in periodontal lesion
Oxidative stress plays a significant role in the pathogenesis of periodontitis. The level of SOD was detected in cases of chronic periodontitis. This enzyme, which is present in the periodontal ligament, neutralizes the action of reactive oxygen species [7].
Role of antioxidants in oral mucosal lesions
The role of this enzyme has been studied in cancer patients, and it has been observed that most tumour cells are deficient in manganese super oxides. Manganese SOD has been found to be a tumour suppressor.
Lichen planus is an autoimmune disease. Evaluation of oxidative stress in lichen planus by evaluation of serum SOD and catalase levels showed increased SOD levels with decreased catalase levels than in the control group. Catalase is the main enzyme in the elimination of peroxides. An imbalance between the antioxidant and free radicals leads to the accumulation of hydrogen peroxide, which leads to the vacuolization of the basal cells seen in histopathological sections of lichen planus.
Role of antioxidants in immune-mediated systemic diseases
Diabetes (Type 1 and Type 2) caused by inflammatory periodontal disease assessed levels of oxidized and reduced glutathione. Glutathione levels in optional saliva were significantly lower than in diabetic controls. Glutathione levels showed an increase with probing depth in both type 1 and type 2 diabetes samples. This supports the fact that free radical generation is increased in chronic hyperglycaemia, leading to an increase in reduced glutathione.
References
- Young IS, Woodside JV. Antioxidants in health and disease. J Clin Pathol 2001; 54(3):176-186.
[Crossref] [Google Scholar] [PubMed]
- Ramasarma T. Many faces of superoxide dismutase, originally known as erythrocuprein. Current Science 2007:184-91.
- Robbins D, Zhao Y. The role of manganese superoxide dismutase in skin cancer. Enzyme Res 2011.
[Crossref] [Google Scholar] [PubMed]
- Oberley LW, Buettner GR. Role of superoxide dismutase in cancer: A review. Cancer Res 1979; 39(4):1141-9.
[Google Scholar] [PubMed]
- Townsend DM, Tew KD, Tapiero H. The importance of glutathione in human disease. Biomed Pharmacother 2003; 57(3-4):145-155.
[Crossref] [Google Scholar] [PubMed]
- Maritim AC, Sanders A, Watkins Iii JB. Diabetes, oxidative stress, and antioxidants: A review. J Biochem Mol Toxicol. 2003; 17(1):24-38.
[Crossref] [Google Scholar] [PubMed]
- Aly DG, Shahin RS. Oxidative stress in lichen planus. Acta Dermatovenerol Alp Pannonica Adriat. 2010; 19(1):3-11.
[Google Scholar] [PubMed]
Copyright: © 2022 The Authors. This is an open access article under the terms of the Creative Commons Attribution NonCommercial ShareAlike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.