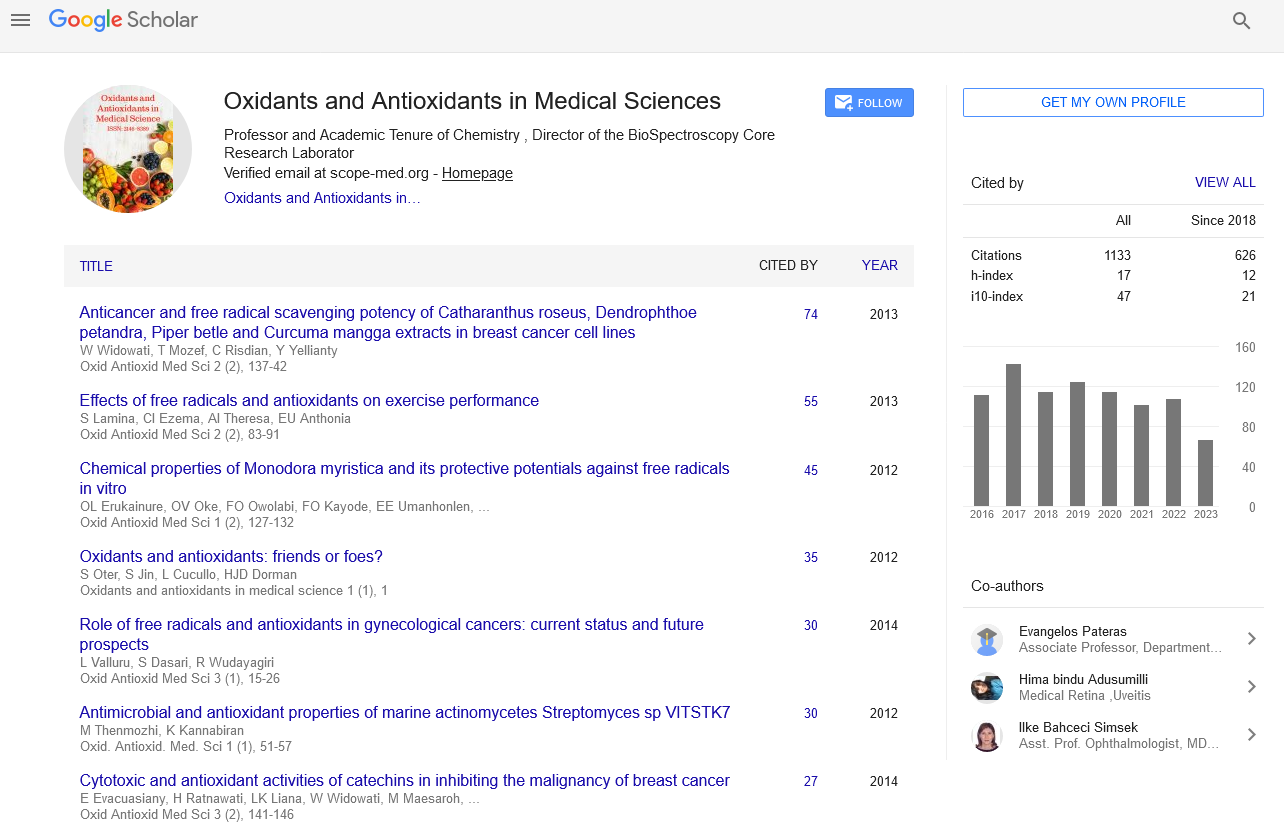
Commentary - Oxidants and Antioxidants in Medical Science (2022)
Significant Role of Antioxidant and Oxidative Stress Markers in Oral Lichen Planus
Mar Morase*Mar Morase, Department of Chemistry, University of Purnea, Purnia, Bihar, India, Email: mar.morase@hotmail.com
Received: 01-Nov-2022, Manuscript No. EJMOAMS-22-79587; Editor assigned: 04-Nov-2022, Pre QC No. EJMOAMS-22-79587 (PQ); Reviewed: 21-Nov-2022, QC No. EJMOAMS-22-79587; Revised: 28-Nov-2022, Manuscript No. EJMOAMS-22-79587 (R); Published: 05-Dec-2022
Description
Oral Lichen Planus (OLP), a chronic inflammatory disease characterized by relapses and remissions, can be found in about 2% of people worldwide, with an overall age-standardized global prevalence of 1.27% (0.96% in men and 1.57% in women) in the general population, it occurs more often in women aged 50 to 60 years. OLP is a precancerous lesion and malignant transformation ranges between 0% and 12.5%. Although its aetiology is unknown, it is thought to be mediated by an immune disorder. Therefore, more extensive knowledge and more accurate diagnostic tools of OLP are particularly important.
In recent years, there has been increasing research interest in Oxidative Stress (OS) in the pathogenesis of several diseases, such as inflammatory, chronic degenerative (Alzheimer’s disease) [1-4], cardiovascular or autoimmune diseases [5-8]. OS modifies the normal intracellular balance, producing excessive oxidants, i.e. Reactive Oxygen Species (ROS) and Reactive Nitrogen Species (RNS), leading to a relative lack of enzymatic and non-enzymatic antioxidants [9,10]. Members of antioxidant systems are currently used as “indirect” biomarkers of oxidative stress [11]. Enzymatic antioxidant systems include Superoxide Dismutase (SOD), Catalase (CAT), and Glutathione Peroxidase (GSHPx) [12,13]. Non-enzymatic antioxidant systems include minerals and vitamins [14].
OS may play a central role in the aetiology of OLP [15]. Sub epithelial infiltration of T lymphocytes in OLP contributes to the local production of cytokines that can stimulate the production of ROS. The presence of apoptosis is a characteristic feature of OLP. ROS are essential mediators of apoptosis and can result in keratinocyte dysfunction and apoptosis.
Oxidative stress markers in Oral Lichen Planus (OLP)
Lipid Peroxidation Malondialdehyde (MDA): Three studies showed significantly higher MDA in serum/ plasma from patients with OLP, while one study reported no difference. Overall, serum/plasma MDA showed a significant increase in OLP with statistically significant heterogeneity. MDA was measured in saliva from OLP in nine studies and was found to be significantly elevated in all nine, with statistically significant heterogeneity.
8-Hydroxy-deoxy (8-OHdG): For evidence of oxidative DNA/RNA damage, 8-OHdG in the saliva of OLP patients was evaluated in two studies (70 patients) and found to be elevated in both based on a random effects model with statistically significant heterogeneity.
Antioxidant Barrier in Oral Lichen Planus (OLP)
Glutathione Peroxidase (GPx): In saliva, all three studies reported significantly lower GPx in OLP cases, while there was no significant association of GPx with OLP in the meta-analyses. In addition, in a single study, serum GPx (30 patients), serum thiol (22 patients), and salivary GSH (62 patients) were determined and found to have decreased levels.
Uric Acid (UA): Plasma/serum UA was investigated in three studies and found to be significantly reduced in OLP compared to controls, with statistically significant heterogeneity. Four studies reported lower salivary UA in OLP cases, while one study reported no statistically significant difference between OLP and controls. Meta- analysis for UA assessed in saliva was -2.65 with statistically significant heterogeneity.
Zinc (Zn): Contrasting data were reported from two studies on serum/plasma Zn levels. Meta-analysis for serum/plasma Zn showed no significant difference between OLP and controls. Only one study evaluated salivary Zn and showed no significant difference between OLP and healthy controls.
Vitamins: Regarding vitamin A, one study with 36 patients with OLP observed no difference, while a large study with 62 patients with OLP detected significantly higher vitamin A content in saliva. Regarding vitamin C, two studies (76 patients) were both conducted that showed lower vitamin C content in saliva from OLP. For vitamin E, two studies (76 patients) observed reduced salivary vitamin E levels, while a single study (62 patients) found no significant difference between OLP patients and controls. Overall, salivary vitamin C levels had a significant decrease in OLP with statistically significant heterogeneity, while there were no significant differences in salivary vitamin E and vitamin A between OLP and controls.
References
- McCartan BE, Healy C. The reported prevalence of oral lichen planus: a review and critique. J Oral Pathol Med. 2008; 37(8):447-453.
[Crossref] [Google scholar] [Pubmed]
- Payeras MR, Cherubini K, Figueiredo MA, Salum FG. Oral lichen planus: focus on etiopathogenesis. Arch Oral Biol. 2013; 58(9):1057-1069.
[Crossref] [Google scholar] [Pubmed]
- Gonzalez-Moles MA, Scully C, Gil-Montoya J. Oral lichen planus: Controversies surrounding malignant transformation. Oral Dis. 2008; 14(3):229-243.
[Crossref] [Google scholar] [Pubmed]
- Scully C, Beyli M, Ferreiro MC, Ficarra G, Gill Y, Griffiths M. Update on oral lichen planus: etiopathogenesis and management. Crit Rev Oral Biol Med. 1998; 9(1):86-122.
[Crossref] [Google scholar] [Pubmed]
- Bhatia V, Sharma S. Role of mitochondrial dysfunction, oxidative stress and autophagy in progression of Alzheimer's disease. J Neurol Sci. 2021; 421:117253.
[Crossref] [Google scholar] [Pubmed]
- Guarneri F, Custurone P, Papaianni V, Gangemi S. Involvement of RAGE and oxidative stress in inflammatory and infectious skin diseases. Antioxidants. 2021; 10(1):82.
[Crossref] [Google scholar] [Pubmed]
- Izzo C, Vitillo P, Di Pietro P, Visco V, Strianese A, Virtuoso N. The role of oxidative stress in cardiovascular aging and cardiovascular diseases. Life. 2021; 11(1):60.
- Wójcik P, Gęgotek A, Žarković N, Skrzydlewska E. Oxidative stress and lipid mediators modulate immune cell functions in autoimmune diseases. Int J Mol Sci. 2021; 22(2):723.
[Crossref] [Google scholar] [Pubmed]
- Miricescu D, Totan A, Calenic B, Mocanu B, Didilescu A, Mohora M. Salivary biomarkers: Relationship between oxidative stress and alveolar bone loss in chronic periodontitis. Acta Odontol Scand. 2014; 72(1):42-47.
[Crossref] [Google scholar] [Pubmed]
- Peluso I, Raguzzini A. Salivary and urinary total antioxidant capacity as biomarkers of oxidative stress in humans. Patholog Res Int. 2016; 2016.
[Crossref] [Google scholar] [Pubmed]
- Dröge W. Free radicals in the physiological control of cell function. Physiol Rev. 2002; 82(1):47-95.
[Crossref] [Google scholar] [Pubmed]
- Abrahams BS, Geschwind DH. Advances in autism genetics: On the threshold of a new neurobiology. Nat Rev Genet. 2008; 9(5):341-355.
[Crossref] [Google scholar] [Pubmed]
- Abrahams BS, Geschwind DH. Connecting genes to brain in the autism spectrum disorders. Arch Neurol. 2010; 67(4):395-359.
[Crossref] [Google scholar] [Pubmed]
- McGinnis WR. Oxidative stress in autism. Altern Ther Health Med. 2004; 10(6):22-36.
[Google scholar] [Pubmed]
- Upadhyay RB, Carnelio S, Shenoy RP, Gyawali P, Mukherjee M. Oxidative stress and antioxidant defense in oral lichen planus and oral lichenoid reaction. Scand J Clin Lab Invest. 2010; 70(4):225-228.
[Crossref] [Google scholar] [Pubmed]
Copyright: © 2022 The Authors. This is an open access article under the terms of the Creative Commons Attribution NonCommercial ShareAlike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.