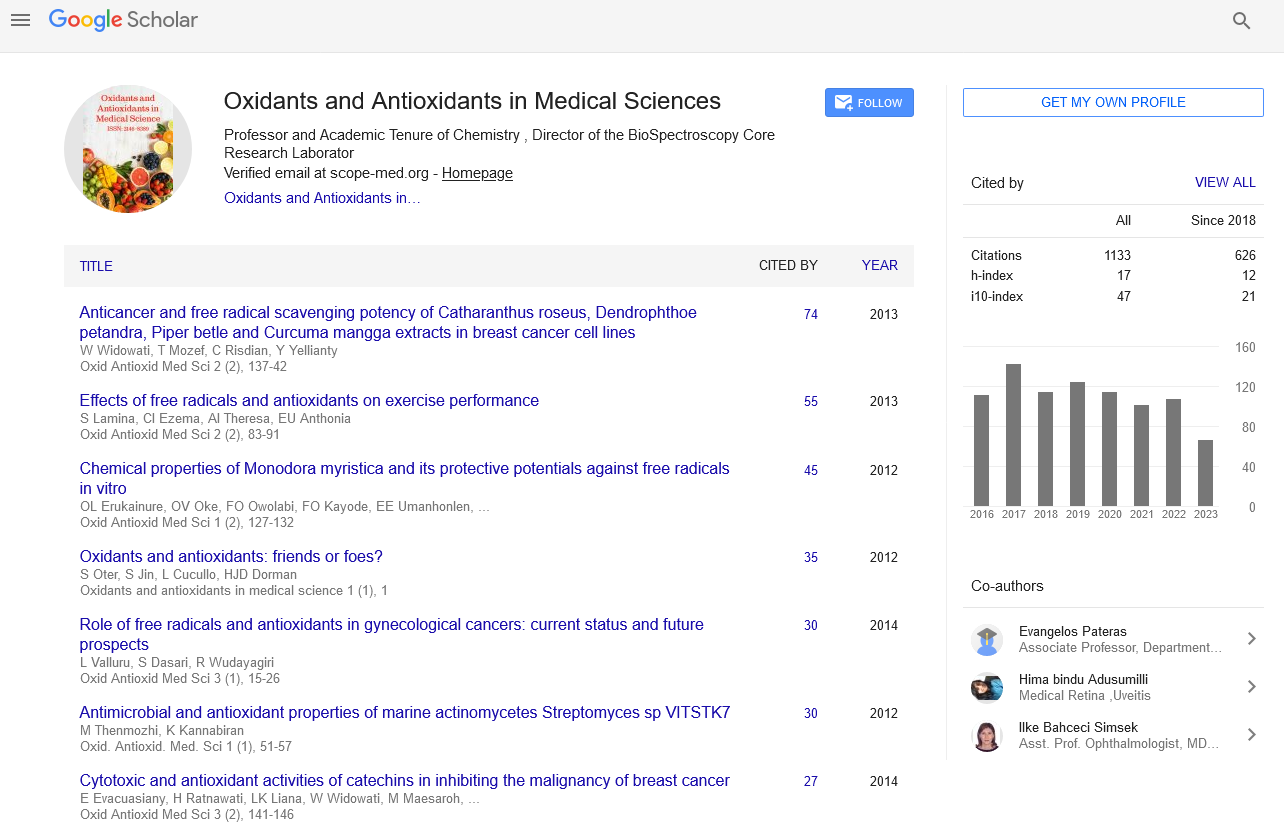
Perspective - Oxidants and Antioxidants in Medical Science (2022)
Types of Cardiovascular Diseases due to Reactive Oxygen Species
Pault Mour*Pault Mour, Department of Chemical Engineering, University of Tehran, Tehran, Iran, Email: pautmour@gmail.com
Received: 01-Nov-2022, Manuscript No. EJMOAMS-22-79584; Editor assigned: 04-Nov-2022, Pre QC No. EJMOAMS-22-79584 (PQ); Reviewed: 21-Nov-2022, QC No. EJMOAMS-22-79584; Revised: 28-Nov-2022, Manuscript No. EJMOAMS-22-79584 (R); Published: 05-Dec-2022
Description
ROS are molecules containing one or more unpaired electrons in their orbital that provide a significant degree of reactivity towards ROS. Reactive Oxygen Species (ROS) have been linked to the pathogenesis of several diseases, including cardiovascular diseases. The presence of increased amounts of ROS has been found to cause damage to major macromolecules in cells including vascular Endothelial Cells (EC) and other cell types in the cardiovascular system, leading to cellular and systemic dysfunction. For example, endothelial dysfunction caused by increased ROS has been shown to contribute to the development of atherosclerosis, hypertension, ischemic heart disease, ischemia-reperfusion injury, and other vascular diseases.
ROS have been reported to affect almost all organs in the body, leading to pathological conditions such as pulmonary fibrosis and vascular retinopathy. Many studies indicate the essential role of antioxidants in improving pathophysiological conditions. Several studies from different groups demonstrated that the reduction of ROS had rather deleterious effects on the cardiovascular system, including endothelial cells [1,2]. Several recent studies have supported a beneficial role of increased ROS in the vasculature, depending on the source and duration of subcellular ROS [3–6].
There are several different intracellular sources of ROS, including Dinucleotide Phosphate (NADPH) oxidases, mitochondria, peroxisomes, lysosomes, xanthine oxidases, cytochrome P450, etc. Originally, ROS-producing enzymes were discovered in phagocytic cells, where large amounts of ROS are produced physiologically by the membrane-bound enzymes NADPH oxidase (NOX) to kill microbes.
Types
Pulmonary and renovascular hypertension: ROS are also involved in renovascular hypertension and chronic pulmonary hypertension associated with hypoxia. In renovascular hypertension, which is caused by increased renal renin release, ROS are thought to impair endothelium- dependent vasorelaxation [7]. The finding that in vivo administration of polyethylene glycol-conjugated superoxide dismutase (PEG-SOD) or in vitro treatment with the antioxidant tirone improved endothelial function in an AngII animal model also supports a critical role for ROS. ROS levels have been found to correlate with the level of hypoxia, which in turn plays an important role in the pathogenesis and development of pulmonary hypertension.
Atherosclerosis and ischemic heart disease: Endothelial dysfunction is one of the initial events that accompany atherosclerosis and coronary heart disease [8]. In conditions predisposing to atherosclerosis, such as hypercholesterolemia, ROS react with Low-Density Lipoproteins (LDL), leading to the formation of oxidized LDL (oxLDL), which is the main effector in the development of atherosclerosis. Increased NADPH oxidase activity and high ROS levels have been reported in atherosclerotic lesions. Increased p22phox subunit expressions along with elevated ROS levels in atherosclerotic lesions of patients with unstable angina have been reported.
Ischemic-reperfusion injury: Ischemic damage to the myocardium causes hypoxia and reduced oxygenation of the area supplied by the stenosis or blocked coronary vessel. It most often occurs in atherosclerosis. Deoxygenated cells are subject to reversible cell damage if the lack of blood is transient or short-term. Cardiac muscle cells are able to withstand ischemia for a maximum of 30 minutes, after which they undergo irreversible injury followed by death by necrosis. Necrotic tissue releases its cellular contents, including enzymes and ROS, into the surrounding environment. Reperfusion at this stage is more harmful than beneficial; simply put, the spread of these toxic substances into the environment causes further damage to the surrounding healthy cells.
Beneficial effects of ROS
Several researchers have hypothesized that stopping the abnormal production of ROS and increasing the natural protective activity of antioxidants may lead to beneficial outcomes in the treatment of cardiovascular disease.
References
- Abid MR, Kachra Z, Spokes KC, Aird WC. NADPH oxidase activity is required for endothelial cell proliferation and migration. FEBS Lett. 2000; 486(3):252-256.
[CrossRef] [Google Scholar] [Pubmed]
- Wang Y, Zang QS, Liu Z, Wu Q, Maass D, Dulan G. Regulation of VEGF-induced endothelial cell migration by mitochondrial reactive oxygen species. Am J Physiol Cell Physiol. 2011; 301(3):C695-704.
[CrossRef] [Google Scholar] [PubMed]
- Kim YM, Kim SJ, Tatsunami R, Yamamura H, Fukai T, Ushio-Fukai M. ROS-induced ROS release orchestrated by Nox4, Nox2, and mitochondria in VEGF signaling and angiogenesis. Am J Physiol Cell Physiol. 2017; 312(6):C749-764.
[CrossRef] [Google Scholar] [PubMed]
- Schröder K, Zhang M, Benkhoff S, Mieth A, Pliquett R, Kosowski J. Nox4 is a protective reactive oxygen species generating vascular NADPH oxidase. Circ Res. 2012; 110(9):1217-1225.
[CrossRef] [Google Scholar] [PubMed]
- Shafique E, Choy WC, Liu Y, Feng J, Cordeiro B, Lyra A. Oxidative stress improves coronary endothelial function through activation of the pro-survival kinase AMPK. Aging. 2013; 5(7):515-530.
[CrossRef] [Google Scholar] [PubMed]
- Craige SM, Chen K, Pei Y, Li C, Huang X, Chen C. NADPH oxidase 4 promotes endothelial angiogenesis through endothelial nitric oxide synthase activation. Circulation. 2011; 124(6):731-740.
[CrossRef] [Google Scholar] [PubMed]
- Jung O, Schreiber JG, Geiger H, Pedrazzini T, Busse R, Brandes RP. gp91phox-containing NADPH oxidase mediates endothelial dysfunction in renovascular hypertension. Circulation. 2004; 109(14):1795-1801.
[CrossRef] [Google Scholar] [PubMed]
- Heitzer T, Schlinzig T, Krohn K, Meinertz T, Münzel T. Endothelial dysfunction, oxidative stress, and risk of cardiovascular events in patients with coronary artery disease. Circulation. 2001; 104(22):2673-2678.
[CrossRef] [Google Scholar] [PubMed]
Copyright: © 2022 The Authors. This is an open access article under the terms of the Creative Commons Attribution NonCommercial ShareAlike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.